Sperm Motility Improvement Timeline: How Long Does It Take to Improve?
Introduction
Male fertility depends heavily on the ability of sperm to move efficiently toward the egg. This movement, known as sperm motility, is as important as sperm count for natural conception. When couples face difficulty conceiving, one of the most common findings on semen analysis is reduced motility. For this reason, many men search for a clear, realistic sperm motility improvement timeline to understand how long recovery may actually take and what factors influence it.
From a clinical perspective, sperm motility reflects the health of the entire sperm production process, including hormone balance, testicular function, and lifestyle habits. According to World Health Organization standards, normal semen should have at least 40 percent motile sperm and 32 percent with progressive forward movement. Values below this range can significantly reduce the chances of pregnancy, even when sperm count appears normal.
The uncertainty surrounding how long it takes to improve motility can create considerable stress for individuals and couples. Some men expect changes within a few weeks, while others are told it may take several months. Both are partially correct, depending on the cause and the interventions used. Because sperm production follows a biological cycle that lasts nearly three months, true improvement usually requires patience, medical evaluation, and consistent lifestyle modifications.
This guide explains the complete sperm motility improvement timeline from a medical standpoint. It also clarifies what changes may occur in the short term versus the long term, what delays recovery, and how treatments, supplements, and lifestyle measures influence results
1. Causes and Risk Factors Affecting Sperm Motility
Understanding the underlying cause of reduced sperm motility is essential for predicting the sperm motility improvement timeline. From a clinical standpoint, low motility, also called asthenozoospermia, is rarely due to a single factor. It is usually the result of a combination of medical, lifestyle, environmental, and sometimes genetic influences. Identifying and correcting these factors early significantly improves the chances of recovery.
1.1 Medical Causes
Several medical conditions directly interfere with normal sperm movement:
- Varicocele: This is the most common correctable cause of low motility. Dilated veins around the testicle raise local temperature and impair sperm function.
- Hormonal Imbalances: Low testosterone, elevated prolactin, or thyroid disorders can disrupt sperm maturation.
- Genital Tract Infections: Prostatitis, epididymitis, and sexually transmitted infections can damage sperm structure and motility.
- Chronic Systemic Diseases: Diabetes, kidney disease, and autoimmune disorders often affect sperm quality.
- Genetic Conditions: Y-chromosome microdeletions and primary ciliary dyskinesia impair sperm movement at a cellular level.
These medical causes often require targeted treatment before any meaningful improvement in motility can occur.
1.2 Lifestyle-Related Risk Factors
Lifestyle choices play a major role in delayed or poor recovery in the sperm motility improvement timeline:
- Cigarette smoking: Reduces oxygen delivery to sperm and increases DNA damage.
- Alcohol consumption: Suppresses testosterone and increases oxidative stress.
- Recreational drugs: Marijuana, anabolic steroids, and opioids are well-known suppressors of sperm motility.
- Obesity: Excess body fat alters estrogen-testosterone balance and increases scrotal temperature.
- Poor diet: Low intake of antioxidants such as zinc, selenium, vitamin C, and omega-3 fatty acids weakens sperm movement.
- Chronic psychological stress: Disrupts hormonal regulation through elevated cortisol levels.
- Sleep deprivation: Alters luteinizing hormone and testosterone secretion patterns.
Patients seeking additional guidance on lifestyle-driven fertility issues can explore educational content at
https://erectileandfertilityguide.com, which addresses interconnected reproductive health topics.
1.3 Environmental and Occupational Factors
Environmental exposure is an increasingly recognized contributor:
- Heat exposure: Frequent hot baths, saunas, prolonged laptop use on the lap, and tight underwear increase testicular temperature.
- Toxins and pollutants: Pesticides, heavy metals, phthalates, and bisphenol-A (BPA) damage sperm mitochondria.
- Radiation exposure: Occupational exposure in certain industries reduces sperm motility over time.
These factors often cause gradual decline and slow recovery unless exposure is eliminated.
1.4 Medications That Lower Sperm Motility
Several commonly used drugs negatively affect sperm movement:
- Testosterone replacement therapy
- Finasteride and dutasteride
- Chemotherapy and radiation therapy
- Certain antidepressants
- Alpha-blockers and antihypertensives
In many cases, motility improves only after medication modification under medical supervision.
1.5 Age-Related Decline
Although men can produce sperm throughout life, sperm motility steadily declines after the age of 40. Mitochondrial dysfunction, DNA fragmentation, and reduced antioxidant defenses are common age-related contributors. This does not prevent improvement but often lengthens the sperm motility improvement timeline.
Table: Common Causes of Low Sperm Motility and Expected Reversibility
| Cause | Reversible | Typical Improvement Timeline |
| Varicocele | Yes (with surgery) | 3–6 months post-repair |
| Smoking | Yes | 2–4 months after quitting |
| Hormonal imbalance | Often | 2–5 months with treatment |
| Infections | Yes | 4–8 weeks after treatment |
| Obesity | Yes | 3–6 months with weight loss |
| Genetic disorders | No | Assisted reproduction required |
| Chemotherapy | Partially | 6–24 months or permanent |
Key Clinical Insight
From a urologist’s perspective, no two patients share the same sperm motility improvement timeline because recovery is entirely dependent on the cause, severity, duration of exposure, and treatment consistency. Patients with correctable lifestyle factors often show improvement within one spermatogenic cycle, while those with structural or genetic issues may require medical or assisted reproductive interventions.
2. Symptoms and Warning Signs of Poor Sperm Motility
2.1 Symptoms of Low Sperm Motility and How They Affect the Sperm Motility Improvement Timeline
From a medical standpoint, one of the most challenging aspects of low sperm motility is that it usually produces no obvious physical symptoms. Most men with impaired motility feel completely normal and discover the issue only during a fertility evaluation. This silent nature is precisely why many patients experience delays in diagnosis and in starting their sperm motility improvement timeline.
Infertility as the Primary Warning Sign
The most common and often the only clinical sign of poor sperm motility is difficulty achieving pregnancy despite regular, unprotected intercourse for 12 months or longer.
- Couples may conceive slowly or not at all.
- Miscarriages may occur due to increased sperm DNA damage associated with poor motility.
- Delayed conception often leads to emotional and psychological stress.
When pregnancy does not occur within the expected timeframe, semen analysis is one of the first tests recommended.
2.2 Absence of Sexual Dysfunction in Most Cases
It is important to clarify a frequent misconception. Low sperm motility does not usually cause erectile dysfunction, low libido, or ejaculation problems. Sexual performance can be entirely normal while fertility is impaired. However, some conditions that affect motility, such as hormonal imbalance or diabetes, may also impact sexual function. Educational material on these interlinked issues is available at
https://erectileandfertilityguide.com.
2.3 Associated Symptoms When an Underlying Disease Is Present
Although motility issues alone are silent, associated medical conditions may produce warning signs:
- Varicocele: Dull scrotal pain, a heavy sensation in the testicles, or visible enlarged veins.
- Infections: Burning during urination, pelvic pain, fever, or abnormal discharge.
- Hormonal disorders: Fatigue, reduced muscle mass, low libido, weight gain, or mood changes.
- Diabetes and systemic illness: Frequent urination, excessive thirst, neuropathy, or unexplained fatigue.
These symptoms do not confirm poor motility but strongly suggest the need for fertility evaluation.
2.4 When to Suspect Sperm Motility Problems
Men should consider testing if any of the following apply:
- Inability to conceive after 12 months of regular intercourse.
- History of testicular surgery, trauma, or infections.
- Long-term smoking, alcohol use, or substance abuse.
- Exposure to heat, radiation, or industrial toxins.
- Use of testosterone or anabolic steroids.
- History of chemotherapy or radiation therapy.
Early testing allows earlier intervention and shortens the sperm motility improvement timeline.
2.5 When to See a Doctor Urgently
Immediate medical consultation is recommended when fertility issues are combined with:
- Sudden testicular pain or swelling
- Rapid testicular shrinkage
- Blood in semen
- Severe erectile or ejaculatory disorders
- Symptoms of systemic disease
These may indicate serious underlying conditions requiring prompt treatment.
Key Clinical Insight
Low sperm motility is typically a laboratory finding rather than a symptomatic disease. Waiting for physical symptoms often delays diagnosis and treatment. From a medical perspective, early semen analysis in couples facing fertility delay is the most effective way to detect motility problems and begin the sperm motility improvement timeline as early as possible.
3. Diagnosis
Accurate diagnosis is the foundation of any successful sperm motility improvement timeline. From a clinical perspective, treatment should never begin without confirming the degree of motility impairment and identifying the underlying cause. A structured diagnostic approach allows us to distinguish temporary, reversible conditions from more persistent medical problems.
3.1 Semen Analysis: The Primary Diagnostic Test
The cornerstone of diagnosis is a semen analysis, performed after 2 to 7 days of sexual abstinence. The sample is evaluated under strict laboratory standards for the following motility parameters:
- Total motility: Percentage of sperm that are moving (normal ≥ 40%)
- Progressive motility: Percentage of sperm moving forward in a straight line (normal ≥ 32%)
- Non-progressive motility: Sperm that move but do not advance
- Immotile sperm: Completely non-moving sperm
Other parameters such as sperm concentration, morphology, vitality, semen volume, and pH are also assessed because these directly influence fertility outcomes.
Because sperm parameters vary naturally, at least two semen analyses, spaced 2 to 3 weeks apart, are required for an accurate diagnosis.
3.2 World Health Organization (WHO) Reference Values
The WHO provides internationally accepted lower reference limits for semen quality. These standards guide clinical decision-making:
| Parameter | Normal Reference Value |
| Total Motility | ≥ 40% |
| Progressive Motility | ≥ 32% |
| Sperm Concentration | ≥ 16 million/mL |
| Total Sperm Count | ≥ 39 million |
| Morphology (Normal Forms) | ≥ 4% |
Values below these thresholds confirm male factor infertility and help determine the expected sperm motility improvement timeline.
3.3 Hormonal Evaluation
If motility is low, hormonal testing is essential to identify endocrine causes. Common tests include:
- Total and free testosterone
- Follicle-stimulating hormone (FSH)
- Luteinizing hormone (LH)
- Prolactin
- Thyroid-stimulating hormone (TSH)
Hormonal imbalances often explain both poor motility and delayed recovery. Correction typically leads to measurable improvement within one to two spermatogenic cycles.
3.4 Scrotal Ultrasound
A scrotal Doppler ultrasound is recommended when physical examination suggests:
- Varicocele
- Testicular atrophy
- Obstruction of the reproductive tract
- Epididymal or testicular masses
Varicocele is the most common surgical cause of low motility and has a well-documented impact on the sperm motility improvement timeline after surgical repair.
3.5 Genetic and Advanced Testing
In severe or long-standing cases, additional tests may be required:
- Karyotyping and Y-chromosome microdeletion testing for genetic infertility
- Sperm DNA fragmentation testing to assess oxidative damage
- Antisperm antibody testing in suspected immune-mediated infertility
These tests are particularly valuable when standard treatments fail to improve motility as expected.
3.6 Frequency of Monitoring During Recovery
During treatment or lifestyle-based recovery, semen analysis is typically repeated:
- Every 3 months during active treatment
- At 6 months if improvement is slow
- After any major intervention such as varicocele surgery or hormonal therapy
Repeating tests too frequently is not useful because sperm production takes approximately 74 to 90 days to complete one full cycle.
3.7 Test Accuracy and Natural Variability
Sperm motility naturally fluctuates due to:
- Recent illness or fever
- Stress
- Changes in sleep patterns
- Temporary toxin exposure
- Variation between laboratories
For this reason, a single abnormal test does not always represent a permanent problem. Clinical interpretation must always consider the full medical context.
For men who also face overlapping sexual health or fertility concerns, additional diagnostic guidance can be found at
https://erectileandfertilityguide.com, which covers interconnected male reproductive conditions.
Key Clinical Insight
From a physician’s standpoint, diagnosing low sperm motility is not simply about identifying an abnormal number. It is about determining why motility is reduced and how reversible the cause is, which directly dictates the length and success of the sperm motility improvement timeline. Accurate diagnosis prevents unnecessary delays and avoids ineffective treatments.
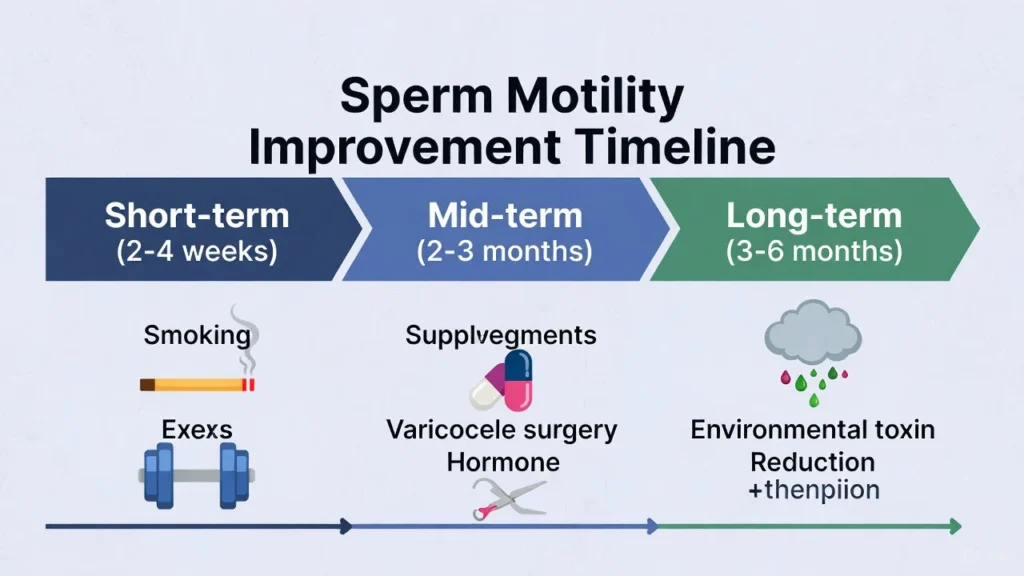
4. Sperm Motility Improvement Timeline
From a medical perspective, the sperm motility improvement timeline is governed by one fundamental biological fact: sperm are produced in cycles. A full cycle of spermatogenesis takes approximately 74 to 90 days, and newly formed sperm then require another 10 to 14 days to mature and gain motility in the epididymis. This means that true, sustained improvement in motility cannot occur overnight, regardless of the treatment used.
However, measurable changes can still appear at different stages depending on the intervention. Below is the realistic, evidence-based timeline physicians use when counseling fertility patients.
4.1 Short-Term Changes: 2 to 4 Weeks
At this stage, structural improvement in sperm motility is minimal, but early biochemical changes begin.
What Can Improve in 2–4 Weeks
- Reduction in oxidative stress after quitting smoking or alcohol
- Improved semen viscosity
- Better seminal fluid quality
- Mild rise in sperm energy metabolism with antioxidant use
- Hormonal stabilization if acute stress or illness was the trigger
What Usually Does Not Improve Yet
- Progressive motility percentage
- Sperm concentration
- Morphology
This phase represents cellular repair, not new sperm production. Patients who expect dramatic motility recovery in a few weeks are usually disappointed, unless the problem was purely transient (such as fever or short-term illness).
4.2 Mid-Term Changes: 2 to 3 Months (One Spermatogenic Cycle)
This is the most critical phase in the sperm motility improvement timeline. By this point, newly produced sperm now reflect all lifestyle changes and medical treatments initiated 8–12 weeks earlier.
Expected Clinical Changes
- 10% to 40% improvement in total and progressive motility in responsive patients
- Reduction in sperm DNA fragmentation
- Improved mitochondrial function
- Better sperm forward progression
- Improved semen volume and vitality
This Timeframe Applies To
- Smoking cessation
- Alcohol withdrawal
- Weight loss
- Treatment of mild infections
- Nutritional supplementation
- Stress normalization
- Controlled diabetes and thyroid disease
Clinical Reality
This is when most men first see objectively meaningful improvement on repeat semen analysis.
4.3 Long-Term Improvement: 3 to 6 Months
Most maximum reversible recovery in sperm motility occurs within this window.
By 6 months, men with correctable causes typically reach their new biological baseline.
What Improves by 3–6 Months
- Peak response to supplementation
- Near-complete benefit from lifestyle correction
- Stable hormonal regulation
- Long-term oxidative stress reduction
- Structural testicular recovery after toxin exposure
This phase is when fertility physicians reassess whether natural conception is realistic or whether assisted reproduction is needed.
4.4 Timeline After Major Interventions
- After Quitting Smoking or Substance Use
- Early cellular repair: 3–4 weeks
- Measurable motility rise: 2–3 months
- Maximum improvement: 4–6 months
Smoking cessation alone can improve progressive motility by up to 20–35% in responsive patients.
- After Varicocele Surgery
- No early improvement expected in first 6–8 weeks
- Initial motility rise: 3 months
- Maximum post-surgical improvement: 6–9 months
Some men continue to improve up to 12 months after repair.
- After Treating Infections
- Symptom relief: 1–2 weeks
- Motility improvement: 4–8 weeks
- Full recovery: 2–3 months
Persistent infections significantly prolong the sperm motility improvement timeline.
- After Stopping Testosterone or Steroids
- Hormonal recovery: 6–12 weeks
- Sperm production restart: 3–6 months
- Full fertility recovery: 6–12 months or longer
4.5 Natural Improvement Timeline With Supplements and Diet
When lifestyle changes and evidence-based supplementation are used together, the average recovery curve is:
- 1 month: Antioxidant levels normalize
- 2–3 months: Noticeable motility improvement
- 4–6 months: Maximum nutritional benefit achieved
Common motility-enhancing supplements include:
- Zinc
- Coenzyme Q10
- L-carnitine
- Selenium
- Omega-3 fatty acids
- Vitamin D
Independent educational resources on fertility-supportive nutrition and male reproductive health are also available at
https://erectileandfertilityguide.com.
4.6 When Improvement Is Slower Than Expected
The sperm motility improvement timeline becomes prolonged when any of the following are present:
- Severe varicocele
- Genetic infertility
- Long-term diabetes
- Persistent obesity
- Continued toxin exposure
- Poor treatment compliance
- Advanced male age
In these cases, assisted reproductive techniques such as IUI, IVF, or ICSI may be recommended instead of waiting for natural recovery.
4.6 Comparative Timeline Table
| Intervention | First Measurable Improvement | Maximum Expected Improvement |
| Smoking cessation | 2–3 months | 4–6 months |
| Alcohol cessation | 2–3 months | 3–6 months |
| Weight loss | 3 months | 6–9 months |
| Varicocele surgery | 3 months | 6–12 months |
| Infection treatment | 1–2 months | 2–3 months |
| Supplements alone | 2–3 months | 4–6 months |
| Steroid cessation | 3–6 months | 6–12 months |
Key Clinical Insight
From a urologist’s standpoint, the sperm motility improvement timeline is never linear. Patients often see fluctuations between tests, temporary plateaus, or delayed responses. The most important predictors of success are cause correction, consistency of lifestyle change, and medical adherence over at least two full spermatogenic cycles.
5. Treatment Options
when lifestyle measures alone are insufficient, medical intervention becomes essential to accelerate or restore the sperm motility improvement timeline. From a clinical perspective, treatment is always individualized and directed at the underlying cause, not just the abnormal motility value. Below are the principal evidence-based medical options used in modern andrology.
5.1 Treating Underlying Medical Conditions
Before prescribing fertility-specific drugs, physicians first correct systemic conditions that impair sperm movement:
- Diabetes control: Normalizing blood glucose reduces oxidative stress and neuropathic damage to sperm.
- Thyroid disorders: Both hypothyroidism and hyperthyroidism suppress motility and respond well to medical correction.
- Obesity-related hormonal imbalance: Weight reduction combined with endocrine therapy improves testosterone-to-estrogen balance.
Timeline Impact:
Motility improvement typically begins within 2 to 4 months once the systemic disorder is controlled.
5.2 Hormonal Therapy
Hormonal treatment is indicated only when laboratory testing confirms endocrine imbalance.
Common Hormonal Treatments
- Clomiphene citrate: Stimulates natural testosterone production
- Human chorionic gonadotropin (hCG): Enhances intratesticular testosterone
- Aromatase inhibitors: Lower estrogen in obese men
⚠️ Direct testosterone replacement therapy is contraindicated in men trying to conceive because it suppresses sperm production.
Timeline Impact:
- Hormonal stabilization: 4–8 weeks
- Measurable motility improvement: 3–5 months
- Peak benefit: 6–9 months
5.3 Antibiotic and Anti-Inflammatory Therapy
Infections of the prostate, epididymis, or seminal vesicles significantly impair motility through inflammatory oxidative damage.
- Targeted antibiotics based on culture
- Anti-inflammatory drugs for chronic prostatitis
- Antioxidant support during treatment
Timeline Impact:
- Symptom resolution: 1–3 weeks
- Motility improvement: 4–8 weeks
- Full recovery: 2–3 months
Untreated or recurrent infections markedly delay the sperm motility improvement timeline.
5.4 Varicocele Repair Surgery
Varicocele is the most common surgically correctable cause of low sperm motility. Surgical options include:
- Microsurgical subinguinal varicocelectomy
- Laparoscopic ligation
- Percutaneous embolization
Clinical Benefits
- Improves testicular oxygenation
- Lowers scrotal temperature
- Reduces oxidative stress
- Enhances Leydig and Sertoli cell function
Timeline Impact:
- No early change in first 6–8 weeks
- Initial improvement: 3 months
- Maximum benefit: 6–12 months
Pregnancy rates significantly improve within the first year after successful repair in appropriately selected patients.
5.5 Medical Antioxidant Therapy
Even when no specific disease is found, many men have idiopathic oxidative stress, which damages sperm mitochondria and reduces forward movement.
Common physician-prescribed combinations include:
- Coenzyme Q10
- L-carnitine
- Selenium
- Zinc
- Vitamin C and E
- Omega-3 fatty acids
These are often used alongside lifestyle correction and not as standalone therapy.
Timeline Impact:
- Early biochemical changes: 4 weeks
- Motility improvement: 2–3 months
- Maximum improvement: 4–6 months
5.6 Assisted Reproductive Techniques (ART)
When motility remains severely impaired or rapid conception is required, medically assisted fertility techniques are indicated.
Intrauterine Insemination (IUI)
Used for mild to moderate motility defects. Processed sperm are placed directly into the uterus.
- Requires some motile sperm
- Often attempted for 3–6 cycles
In Vitro Fertilization (IVF)
Used when motility is poor and natural fertilization is unlikely.
Intracytoplasmic Sperm Injection (ICSI)
A single sperm is injected directly into the egg. This bypasses virtually all motility barriers and is the gold standard for severe asthenozoospermia.
Timeline Impact:
- Bypasses natural sperm motility improvement timeline
- Pregnancy possible within 1–2 treatment cycles
For couples exploring both natural recovery and assisted options, detailed fertility planning guidance is available through
https://erectileandfertilityguide.com.
5.7 Success Rates and Clinical Limitations
- Medical and surgical treatment is most effective in reversible causes.
- Genetic and severe idiopathic cases respond poorly to medications.
- Delayed diagnosis reduces treatment effectiveness.
- Compliance with treatment and lifestyle change directly determines outcome.
Medical Treatment vs Expected Motility Response
| Treatment | Suitable For | First Response | Maximum Response |
| Hormonal therapy | Endocrine imbalance | 3 months | 6–9 months |
| Antibiotics | Infections | 1–2 months | 2–3 months |
| Varicocele surgery | Clinical varicocele | 3 months | 6–12 months |
| Antioxidants | Idiopathic low motility | 2–3 months | 4–6 months |
| IUI/IVF/ICSI | Severe motility | Immediate | Per cycle |
Key Clinical Insight
From a urologist’s standpoint, medical therapy improves sperm motility only when the underlying pathology is accurately identified. Empirical treatment without proper diagnosis wastes valuable time and often prolongs the sperm motility improvement timeline unnecessarily. Early specialist evaluation offers the highest probability of both natural and assisted conception.
6. Natural Ways to Improve Sperm Motility Faster
From a clinical standpoint, natural interventions form the foundation of any successful sperm motility improvement timeline, regardless of whether medical treatment is also required. These measures target oxidative stress, mitochondrial dysfunction, hormonal imbalance, and testicular heat exposure, which are the most common reversible causes of reduced motility. When followed consistently, natural strategies can produce measurable improvement within one spermatogenic cycle.
6.1 Evidence-Based Supplements for Sperm Motility
Multiple clinical trials confirm that targeted micronutrient therapy improves sperm energy production and forward movement by reducing oxidative damage to the sperm tail and mitochondria.
Core Supplements With Proven Benefit
- Zinc (15–30 mg/day): Essential for testosterone synthesis and sperm tail development
- Coenzyme Q10 (100–300 mg/day): Enhances mitochondrial energy for forward progression
- L-carnitine (1–3 g/day): Improves sperm fuel utilization and motility velocity
- Selenium (100–200 mcg/day): Protects sperm from oxidative damage
- Omega-3 fatty acids (1–2 g/day): Improves sperm membrane flexibility
- Vitamin D: Supports testosterone regulation and sperm maturation
- Vitamin C and E: Potent antioxidant protection
Expected Timeline With Consistent Use
- 4 weeks: Reduction in oxidative stress markers
- 2–3 months: Measurable rise in progressive motility
- 4–6 months: Peak supplement-related benefit
Supplements are most effective when combined with dietary and lifestyle correction rather than used alone.
6.2 Fertility-Supportive Diet for Faster Recovery
Dietary patterns directly influence sperm mitochondria, DNA integrity, and antioxidant capacity. The most evidence-supported pattern is the Mediterranean-style diet.
Foods That Improve Motility
- Fatty fish (salmon, sardines)
- Eggs and lean poultry
- Leafy green vegetables
- Citrus fruits and berries
- Nuts and seeds
- Whole grains
- Olive oil
- Legumes
Foods That Delay the Sperm Motility Improvement Timeline
- Processed meats
- Trans fats
- Sugary beverages
- Refined carbohydrates
- Excess caffeine
- Highly processed fast foods
Dietary Timeline
- 4–6 weeks: Improved seminal antioxidant environment
- 2–3 months: Improvement in progressive motility
- 3–6 months: Stabilization at higher motility baseline
For additional fertility-focused nutrition guidance, patient education resources are available at
https://erectileandfertilityguide.com.
6.3 Exercise and Physical Activity
Moderate, consistent exercise improves insulin sensitivity, testosterone levels, and testicular blood flow.
Recommended Exercise Pattern
- 30–45 minutes of brisk walking, cycling, or swimming
- 4–5 days per week
- Light resistance training 2–3 days per week
What to Avoid
- Excessive endurance training
- Heavy anabolic steroid use
- Overtraining without recovery
Timeline Effect
- Hormonal improvement: 4–8 weeks
- Motility improvement: 2–4 months
6.4 Heat Protection for the Testicles
Sperm production is extremely temperature sensitive. Even small increases in scrotal temperature can reduce sperm motility dramatically.
Key Preventive Measures
- Avoid hot tubs, saunas, and steam rooms
- Do not place laptops directly on the lap
- Wear loose-fitting cotton underwear
- Avoid prolonged sitting without breaks
Heat-related recovery often shows improvement within 1 to 2 spermatogenic cycles once exposure stops.
6.5 Stress Reduction and Sleep Optimization
Chronic psychological stress suppresses gonadotropin-releasing hormone (GnRH), leading to downstream testosterone reduction and impaired spermatogenesis.
Effective Strategies
- Daily relaxation techniques
- Controlled breathing exercises
- Cognitive behavioral therapy when anxiety is significant
- 7–8 hours of uninterrupted sleep per night
- Consistent sleep-wake schedule
Patients with chronic stress often experience delayed response in their sperm motility improvement timeline until cortisol levels normalize.
6.6 Alcohol, Smoking, and Toxin Avoidance
These remain the most critical lifestyle factors affecting sperm motility worldwide.
- Smoking causes mitochondrial poisoning and DNA fragmentation
- Alcohol suppresses testosterone and increases estrogen
- Environmental toxins impair Sertoli cell function
Recovery After Cessation
- 1 month: Improved seminal plasma quality
- 2–3 months: Improvement in progressive motility
- 4–6 months: Maximum benefit in responsive individuals
6.7 Expected Natural Improvement Timeline (Checklist)
| Natural Strategy | First Response | Maximum Benefit |
| Supplements | 2–3 months | 4–6 months |
| Diet optimization | 2–3 months | 3–6 months |
| Exercise | 2–4 months | 4–6 months |
| Heat avoidance | 1–2 months | 3–4 months |
| Stress reduction | 1–2 months | 3–6 months |
| Smoking cessation | 2–3 months | 4–6 months |
Clinical Caveat
Natural strategies significantly enhance the sperm motility improvement timeline in men with lifestyle-driven or idiopathic low motility. However, they cannot correct genetic disorders, severe varicocele, or advanced testicular failure. In such cases, natural measures should be viewed as supportive rather than curative.
7. Lifestyle and Prevention
From a preventive medicine perspective, long-term lifestyle optimization is the most reliable way to protect gains already achieved in the sperm motility improvement timeline and prevent future decline. Many men experience short-term improvement with treatment but relapse within months due to unresolved lifestyle risks. Sustainable habits are therefore central to lasting fertility health.
7.1 Smoking Cessation as a Permanent Fertility Strategy
Long-term tobacco exposure causes persistent mitochondrial damage, sperm DNA fragmentation, and microvascular impairment of the testes.
Preventive Benefits of Permanent Smoking Cessation
- Sustains improved progressive motility
- Reduces sperm DNA damage
- Lowers miscarriage risk
- Improves natural conception rates
Men who resume smoking after recovery frequently experience a decline in motility within 3–6 months, reversing prior therapeutic gains.
7.2 Alcohol Moderation for Hormonal Stability
Chronic alcohol intake suppresses hypothalamic-pituitary-gonadal axis function. Even moderate excess intake can reduce testosterone and elevate estrogen.
Fertility-Safe Alcohol Limits
- No more than 1–2 standard drinks per week
- Complete avoidance during active fertility recovery
Long-term abstinence or strict moderation helps stabilize hormonal support for sustained sperm motility.
7.3 Weight Management and Metabolic Health
Obesity increases testicular temperature, estrogen production, insulin resistance, and systemic inflammation. All these factors suppress sperm motility over time.
Preventive Targets
- Body mass index below 25
- Waist circumference under 40 inches
- Fasting glucose and lipid profile within normal range
Sustained weight control protects long-term spermatogenic function and reduces relapse after initial recovery.
7.4 Environmental and Occupational Toxin Prevention
Many patients unknowingly re-expose themselves to fertility-damaging toxins after treatment.
High-Risk Exposures to Avoid Long-Term
- Pesticides and herbicides
- Heavy metals such as lead and mercury
- Industrial solvents
- Plastic-derived endocrine disruptors (BPA, phthalates)
Practical Prevention
- Use protective equipment at work
- Store food in glass rather than plastic
- Filter drinking water
- Avoid heated plastic containers
Environmental control is especially critical for men with previously unexplained low motility.
7.5 Long-Term Heat Protection
Testicular temperature regulation must be maintained permanently, not just during active treatment.
Daily Preventive Measures
- Avoid prolonged sitting without breaks
- Use standing desks when possible
- Avoid tight underwear consistently
- Limit sauna and steam room exposure
Men who relapse into chronic heat exposure frequently show motility decline within one spermatogenic cycle.
7.6 Medication Awareness and Fertility Preservation
Certain medications permanently or temporarily impair sperm production and movement.
Drugs Requiring Fertility Counseling
- Testosterone replacement
- Anabolic steroids
- Chemotherapy agents
- Some antidepressants and antihypertensives
Before initiating long-term therapy with fertility-toxic drugs, sperm cryopreservation should be discussed. This is a critical preventive strategy for men at risk of future infertility.
7.7. Long-Term Preventive Checklist
| Preventive Action | Long-Term Fertility Benefit |
| Permanent smoking cessation | Maintains improved motility and DNA quality |
| Alcohol moderation | Stable testosterone levels |
| Healthy weight maintenance | Lower estrogen and inflammation |
| Toxin avoidance | Protects Sertoli cell function |
| Heat protection | Preserves sperm maturation |
| Medication review | Prevents iatrogenic fertility loss |
| Regular follow-up | Early detection of relapse |
7.8 Ongoing Fertility Monitoring
From a clinical perspective, men with a history of low sperm motility should:
- Repeat semen analysis every 6–12 months
- Monitor testosterone levels when metabolic disease is present
- Maintain follow-up with a fertility specialist when attempting conception
Key Clinical Insight
The sperm motility improvement timeline does not end with recovery. Without sustained preventive habits, relapse is common. Lifelong fertility protection requires continuous management of metabolic health, environmental exposure, and hormonal balance. Prevention is therefore not an optional step but a permanent component of male reproductive care.
8. When the Timeline Is Delayed
In clinical practice, not all patients follow the typical sperm motility improvement timeline despite excellent compliance with treatment and lifestyle modification. When expected improvement does not occur within 3 to 6 months, it usually indicates the presence of deeper biological limitations or ongoing hidden risk factors. Identifying these delays early prevents prolonged emotional stress and unnecessary waiting.
8.1 Severe or Long-Standing Varicocele
Mild varicoceles often respond well to surgery, but large or long-standing varicoceles may have already caused permanent testicular damage.
Why Recovery Is Delayed
- Chronic hypoxia to testicular tissue
- Irreversible Sertoli cell dysfunction
- Prolonged oxidative stress
Clinical Impact:
Even after successful varicocele repair, improvement may be minimal or require 9–12 months, and in some cases, motility may not normalize.
8.2 Genetic and Chromosomal Disorders
Genetic abnormalities are a major cause of delayed or absent recovery.
Common genetic factors include:
- Y-chromosome microdeletions
- Klinefelter syndrome (47,XXY)
- Primary ciliary dyskinesia
Clinical Impact:
These conditions impair sperm tail structure and movement at a cellular level. As a result, natural improvement in motility is usually not possible, regardless of supplements or lifestyle change. In such cases, assisted reproduction, particularly ICSI, becomes the primary option.
8.3 Chronic Systemic Illness
Long-standing medical conditions reduce sperm quality through hormonal and microvascular mechanisms.
- Poorly controlled diabetes
- Chronic kidney disease
- Liver cirrhosis
- Autoimmune diseases
- Long-standing thyroid disorders
Why the Timeline Is Prolonged
- Persistent oxidative stress
- Ongoing hormonal disruption
- Reduced testicular perfusion
Motility improvement often remains partial and slow, even after aggressive disease control.
8.4 Persistent Toxin Exposure
Many men unknowingly continue to be exposed to fertility-toxic substances despite treatment:
- Industrial chemicals
- Pesticides
- Heavy metals
- Endocrine-disrupting plastics
Even low-level, continuous exposure can completely override the benefits of medical and natural therapy, leading to repeated treatment failure.
8.5 Poor Treatment Compliance
From a physician’s standpoint, non-adherence is one of the most common hidden causes of delayed recovery.
Examples include:
- Inconsistent supplement use
- Continued smoking or alcohol intake
- Skipping medications
- Irregular sleep cycles
- Non-attendance at follow-up visits
Sperm production is extremely sensitive to cumulative exposure. Even small lapses can postpone meaningful improvement by an entire spermatogenic cycle.
8.6 Advanced Male Age
After the age of 40, sperm motility declines due to:
- Mitochondrial dysfunction
- Increased DNA fragmentation
- Reduced antioxidant defense
- Slower cellular regeneration
Although improvement is still possible, the sperm motility improvement timeline is often extended, and the degree of recovery is usually modest compared to younger men.
7.7 When Assisted Reproductive Treatment Becomes Necessary
Medical guidelines suggest considering assisted reproduction when:
- Motility remains severely impaired after 6–9 months of optimized therapy
- Genetic infertility is confirmed
- Female partner age is advanced
- There is significant sperm DNA damage
- Rapid conception is medically necessary
At this stage, further waiting for natural improvement often reduces overall pregnancy success.
Warning Signs That the Timeline Is Stalled
Men should seek reassessment if any of the following occur:
- No improvement after two consecutive semen analyses over 6 months
- Progressive decline in motility despite treatment
- Development of new testicular pain or shrinkage
- Rising FSH levels (indicating testicular failure)
Conclusion
Improving sperm motility is a gradual process influenced by lifestyle, medical conditions, and individual physiology. Most men can expect to see measurable improvements in motility within 2–3 months after implementing targeted interventions, as sperm development cycles take roughly 74 days. Medical treatments, such as hormone therapy or supplements, combined with lifestyle changes—like quitting smoking, reducing alcohol intake, managing stress, and maintaining a balanced diet—can significantly enhance sperm health. Tracking progress through regular semen analysis helps ensure interventions are effective and allows for timely adjustments. By understanding the sperm motility improvement timeline and committing to evidence-based strategies, men can optimize fertility potential and support overall reproductive health.
FAQs
- How long does it take to improve sperm motility naturally?
Most men see noticeable improvements in sperm motility after 2–3 months of lifestyle changes due to the natural sperm production cycle. - Can supplements really help sperm motility?
Yes, supplements containing zinc, selenium, L-carnitine, CoQ10, and vitamin D have been shown to support sperm motility, especially when combined with a healthy lifestyle. - Does quitting smoking improve sperm motility?
Absolutely. Smoking reduces sperm quality, including motility. Improvement may be observed within 2–3 months after quitting. - How often should I get a semen analysis to track improvement?
A repeat semen analysis every 2–3 months is recommended to monitor changes in motility and overall sperm quality. - Can diet impact sperm motility?
Yes, diets rich in antioxidants, omega-3 fatty acids, fruits, and vegetables improve sperm motility, while excessive processed foods and trans fats can impair it. - Are there medical treatments for low sperm motility?
Doctors may recommend hormonal therapy, antioxidants, or assisted reproductive techniques depending on the underlying cause. Consulting a fertility specialist is advised. - Does age affect sperm motility improvement?
Sperm quality naturally declines with age, but men under 40 typically respond better to interventions. Lifestyle improvements still offer benefits at any age. - How can stress management help sperm motility?
Chronic stress negatively impacts hormones regulating sperm production. Techniques like meditation, exercise, and proper sleep can enhance motility.
References
- Erectile and Fertility Guide – Fertility and reproductive health insights.
Website: https://erectileandfertilityguide.com - Effect of oxidative stress on male reproduction — A. Agarwal et al. (2014). World Journal of Men’s Health 32(1):1–17. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC4026229/ (PMC)
- Reduction of sperm DNA damage by oral antioxidant treatment — E. Greco et al. (2005). Journal of Andrology 26(3): 349–353. Abstract available at: https://pubmed.ncbi.nlm.nih.gov/15867002/ (PubMed)
- Role of reactive oxygen species in male infertility — R. K. Sharma & A. Agarwal (1996). Urology 48(6): 835–850. Abstract available at: https://pubmed.ncbi.nlm.nih.gov/8973665/ (PubMed)
- World Health Organization (2021). WHO Laboratory Manual for the Examination and Processing of Human Semen. WHO publication.
— The manual can be accessed via WHO’s publications page: https://www.who.int/publications/i/item/9789240030787