How Long Sperm Improves After Varicocele Surgery: A Doctor’s Complete Fertility Guide
Introduction
Many men undergoing varicocelectomy often ask the same essential question: how long sperm improves after varicocele surgery, and what they should expect during the recovery journey. As a doctor who frequently treats patients with varicocele-related infertility, I see how deeply this question affects couples trying to conceive. Varicocele repair isn’t just a surgical procedure—it marks the beginning of a transformative process for testicular health, sperm regeneration, and overall male fertility.
Before surgery, varicocele causes increased scrotal heat, oxidative stress, and impaired blood flow, all of which directly reduce sperm count, motility, morphology, and even DNA integrity. After surgical correction, the testicles finally return to a healthier environment—but sperm improvement follows a timeline that depends on biology, healing rates, and individual health factors.
This guide will walk you through the complete journey—from what happens immediately after surgery to the months when sperm quality begins to rise.
1. Understanding Varicocele & Its Impact on Sperm Production
A varicocele is essentially an abnormal dilation of the veins within the scrotum, leading to increased heat, impaired blood flow, and chronic oxidative stress around the testicles. These changes gradually damage the cells responsible for sperm production—called Sertoli and Leydig cells—and directly influence how long sperm improves after varicocele surgery, because recovery depends on how much injury existed before repair.
From a clinical standpoint, varicocele is the most common correctable cause of male infertility. Studies show that up to 40% of men with primary infertility have a varicocele, and many experience semen abnormalities long before symptoms become noticeable. Understanding the underlying mechanism helps patients appreciate why sperm improvement does not happen overnight.
How Varicocele Impacts Sperm Quality
Varicocele impairs sperm parameters in several ways:
- Increased scrotal temperature
Elevated heat disrupts spermatogenesis and reduces overall sperm output. - Venous reflux & poor oxygenation
Stagnant blood flow increases oxidative toxins, harming testicular tissue. - Oxidative stress & sperm DNA fragmentation
One of the leading causes of poor sperm motility and abnormal forms. - Hormonal imbalance
Varicocele can reduce testosterone production, further impairing fertility.
These biological disturbances explain why semen quality improves only after the testicular environment normalizes post-surgery.
Why Sperm Improves After Varicocele Surgery
Varicocele repair (microsurgical, laparoscopic, or embolization) restores healthier blood flow, reduces temperature, and lowers oxidative stress. When this happens:
- Testicular cells begin functioning more efficiently
- Sperm DNA damage declines
- Testosterone levels may increase
- Sperm production cycles normalize (approximately 74 days per cycle)
This is why the timeline of improvement is gradual—and why most men see measurable progress only after a full sperm production cycle has passed.
For further reading on male fertility improvement strategies, you can explore additional clinical insights on erectileandfertilityguide.com.”
2. Symptoms & Signs Before Surgery That Influence Post-Operative Sperm Improvement
Before we understand how long sperm improves after varicocele surgery, it is important to recognize the symptoms and signs men typically experience before the procedure. These symptoms often reflect the underlying impact of varicocele on sperm production, testicular function, and overall reproductive health. The severity and duration of these symptoms can directly influence how quickly the testicles recover after repair.
Common Symptoms Men Experience Before Varicocele Surgery
2.1 Dull, Aching Scrotal Pain
Many men report a persistent heaviness or aching sensation in the scrotum, especially:
- After prolonged standing
- After exercise
- By the end of the day
This discomfort is caused by venous congestion and increased scrotal temperature—both of which impair sperm production.
2.2 Noticeable Vein Enlargement
A “bag of worms” appearance on the scrotum is the most classic sign of varicocele.
This visible vein dilation indicates long-standing venous reflux, which negatively affects sperm morphology and motility.
2.3 Reduced Semen Quality
Before surgery, men may experience:
- Low sperm count
- Poor motility
- Abnormal sperm shape (teratozoospermia)
- Low semen volume
- High sperm DNA fragmentation
These changes reflect the unhealthy testicular environment. The more severe these abnormalities, the longer it may take for sperm parameters to improve after varicocele repair.
2.4 Testicular Shrinkage (Atrophy)
Chronic varicocele can lead to loss of testicular volume due to damage to the seminiferous tubules.
Men with testicular atrophy may still improve after surgery, but the recovery timeline is usually extended.
2.5 Hormonal Imbalances
Varicocele can affect Leydig cell function, resulting in:
- Lower testosterone levels
- Elevated FSH
- Reduced inhibin B
Hormonal imbalance often correlates with delayed sperm recovery because hormonal regulation plays a central role in spermatogenesis.
2.6 Impaired Sexual Function
While varicocele does not directly cause erectile dysfunction, many men experience:
- Reduced libido
- Fatigue
- Reduced sexual confidence
These are often secondary to low testosterone or long-standing discomfort. With hormonal improvement after surgery, sexual well-being often improves gradually.
Why These Symptoms Matter for Sperm Recovery
Symptoms and pre-operative findings provide valuable insight into:
- The extent of testicular damage
- Expected sperm improvement timeline
- Individual variability in recovery
For example, a man with severe pain, low testosterone, and high DNA fragmentation may need 6–12 months to see optimal improvement, while someone with mild varicocele and normal hormones may notice improvements within 3 months.
For more male health insights, expert articles on erectileandfertilityguide.com explain how symptoms correlate with fertility outcomes.
3. Causes Affecting Sperm Recovery After Varicocele Surgery
Understanding the causes and risk factors behind delayed sperm improvement helps men set realistic expectations about how long sperm improves after varicocele surgery. Although repairing the varicocele restores a healthier testicular environment, individual biology, age, lifestyle, and pre-existing damage determine how quickly sperm parameters recover.
Primary Causes of Varicocele
Varicocele typically develops due to:
- Defective venous valves
This leads to blood pooling and increased pressure around the testicles. - Left-sided anatomical vulnerability
Most men develop varicocele on the left side due to vein structure and drainage patterns. - Venous reflux
Backward blood flow increases scrotal temperature and oxidative stress.
These foundational causes contribute to longstanding testicular damage, which can influence the recovery timeline after surgery.
Risk Factors That Influence Sperm Recovery After Surgery
Some men experience faster sperm improvement, while others take longer. These differences often relate to the following:
3.1 Severity & Duration of Varicocele
Long-standing or high-grade varicoceles cause more cellular damage.
Men with Grade 3 varicocele may require 6–12 months for significant sperm improvement.
3.2 Age
Younger men often show faster recovery because their testicular tissue is more responsive.
Men over 35 may experience a slower improvement curve.
3.3 Pre-existing Hormonal Imbalances
Low testosterone, elevated FSH, or reduced inhibin-B levels may delay response after surgery.
3.4 Sperm DNA Fragmentation
High DNA fragmentation levels need time to decline even after the varicocele is repaired.
Antioxidant therapy may help accelerate recovery.
3.5 Lifestyle Factors
Habits that affect testicular health can delay sperm improvement:
- Smoking
- Alcohol excess
- Chronic heat exposure (saunas, hot tubs, laptops on lap)
- Stress
- Obesity
- Poor sleep patterns
3.6 Medical Conditions
Certain conditions can slow improvement:
- Diabetes
- Thyroid disorders
- Varicocele recurrence
- Testicular atrophy
- Past scrotal infections or surgeries
3.7 Surgical Technique Used
Microsurgical varicocelectomy offers the highest improvement rates and lowest recurrence, leading to faster recovery compared to laparoscopic or embolization techniques.
Why Risk Factors Matter
All these factors combined explain why two men undergoing the same surgery may experience different recovery timelines. For some, sperm quality starts improving within 3 months, while others may need 9–12 months for optimal results.
4. Diagnosis & Pre-Surgery Tests That Predict How Long Sperm Improves After Varicocele Surgery
Before undergoing varicocelectomy, proper diagnosis and testing play a critical role in determining how long sperm improves after varicocele surgery and what level of improvement a patient can expect. These tests help assess the severity of damage, hormonal balance, DNA integrity, and overall testicular function. A thorough diagnostic approach ensures that surgery is medically justified and that expectations are realistic.
4.1 Semen Analysis (SA) — The Most Important Test
This is the foundational test to evaluate a man’s reproductive health.
A standard semen analysis reports:
- Sperm count
- Motility (progressive & total)
- Morphology
- Semen volume
- pH and viscosity
Varicocele often affects all these parameters, but particularly motility and morphology.
A severely abnormal semen analysis before surgery may indicate that sperm needs multiple production cycles (3–6 months) to show significant improvement after the repair.
What Semen Analysis Predicts:
- The degree of pre-existing damage
- The expected timeline of recovery
- Whether improvement will be mild, moderate, or substantial
Men with mild abnormalities may see improvement within 3 months, while those with severe oligoasthenoteratozoospermia may need 6–12 months.
4.2 Scrotal Ultrasound With Doppler
Ultrasound is used to:
- Confirm varicocele
- Measure vein diameter
- Assess blood reflux
- Evaluate testicular volume
Doppler findings such as high-grade reflux or reduced testicular size correlate with longer sperm recovery time after surgery.
What it tells us:
- Varicocele severity
- Risks of delayed improvement
- Potential need for early intervention
4.3 Hormonal Profile
Hormones regulate spermatogenesis. Testing typically includes:
- FSH – Elevated levels indicate impaired sperm production
- LH
- Total Testosterone
- Prolactin
- Estradiol
- Inhibin-B – A key marker of Sertoli cell function
Hormone Clues for Recovery
- Low testosterone → May delay sperm improvement
- High FSH → Suggests pre-existing testicular injury
- Low inhibin-B → Indicates reduced sperm-producing capacity
Correcting hormonal imbalance post-surgery can accelerate recovery.
4.4 Sperm DNA Fragmentation Test (DFI)
Varicocele is strongly associated with high oxidative stress and DNA fragmentation.
A DFI test measures the percentage of sperm with broken or damaged DNA.
Why this test matters:
- High DFI indicates severe oxidative injury
- DFI often takes 3–6 months to decline after varicocele surgery
- Lower DFI improves natural conception rates and IVF/ICSI outcomes
Antioxidants are often prescribed alongside surgery to speed up DNA repair.
4.5 Testicular Function Assessment
Some men may require additional tests when:
- They have long-standing infertility
- Testicular atrophy is suspected
- Hormone levels are abnormal
Advanced assessments may include:
- Testicular elastography
- Semen oxidative stress markers
- Reactive oxygen species (ROS) testing
These tests predict how quickly testicular health will stabilize post-surgery.
4.6 When Varicocele Surgery Is Medically Indicated
A varicocelectomy is generally recommended when:
- A patient has infertility
- Semen analysis is abnormal
- Varicocele is clinically palpable
- Testicular discomfort persists
- Sperm DNA fragmentation is high
- There is testicular atrophy
- A couple is trying to conceive without success
If multiple tests show significant impairment, the improvement timeline may be longer but still meaningful after surgery.
5. Treatment Options
Many patients want to know how long sperm improves after varicocele surgery, but equally important is understanding what treatments can accelerate this improvement. While varicocelectomy corrects the underlying venous issue, improving sperm parameters still requires time—typically 3 to 6 months for measurable changes and up to 12 months for optimal results.
During this recovery window, several medical and natural treatment strategies can help enhance sperm quality, promote hormonal balance, and support healthier spermatogenesis.
5.1 Antioxidant Therapy (First-Line After Surgery)
Varicocele is strongly associated with high oxidative stress and sperm DNA damage. After repair, restoring DNA integrity is essential for improving count, motility, and morphology.
Common Antioxidants Used Post-Surgery
- Coenzyme Q10 (CoQ10)
- Vitamin C
- Vitamin E
- L-Carnitine
- N-acetyl cysteine (NAC)
- Zinc
- Selenium
Benefits
- Reduces sperm DNA fragmentation
- Improves progressive motility
- Enhances mitochondrial function
- Supports faster recovery of sperm cycles
Most patients see noticeable improvement in 2–3 months when antioxidants are added consistently.
5.2 Hormone Optimization
Hormones play a central role in testicular recovery, especially if pre-surgery tests showed imbalances.
When Hormonal Support Is Needed
- Low testosterone
- High FSH
- Low inhibin-B
- Low LH
- Symptoms of low libido, fatigue, reduced vitality
Possible Treatments
- Clomiphene citrate (Clomid)
- hCG therapy
- Aromatase inhibitors (like anastrozole) when estrogen is high
- Vitamin D supplementation (supports testosterone production)
Correcting hormonal imbalance often reduces the time it takes for sperm to improve after varicocele surgery.
5.3 Supplements for Spermatogenesis Support
Beyond antioxidants, certain supplements directly support sperm formation:
- Folic acid
- Omega-3 fatty acids (DHA/EPA)
- Ashwagandha (clinically shown to increase motility and testosterone)
- Myo-inositol
- Shilajit (purified form)
- L-arginine for improved microcirculation
These agents help create a healthier testicular environment and support each stage of the sperm production cycle.
5.4 Lifestyle Modifications
Lifestyle changes play a significant role in determining how long sperm improves after varicocele surgery.
Key Changes Include:
- Stop smoking
- Limit or eliminate alcohol
- Reduce scrotal heat exposure (hot tubs, saunas, laptops)
- Maintain a healthy BMI
- Increase moderate exercise
- Improve sleep quality
- Manage stress through meditation, yoga, or breathing exercises
These habits can shorten the recovery timeline and significantly enhance semen parameters.
5.5 Diet to Support Sperm Production
Nutrients crucial for sperm growth include:
- Protein-rich foods
- Fresh fruits & vegetables
- Antioxidant-dense foods (berries, nuts)
- Leafy greens
- Whole grains
- Healthy fats (olive oil, avocado)
- Seafood (rich in omega-3)
A fertility-friendly diet helps reduce oxidative stress and supports testicular repair.
5.6 Repeat Semen Analysis Monitoring
After surgery, semen analysis is typically recommended at:
- 3 months
- 6 months
- 9–12 months
Tracking progress helps identify whether sperm improvement is following the expected pattern or if additional interventions are needed.
5.7 When Assisted Reproductive Techniques (ART) Are Recommended
If sperm parameters do not improve adequately within 6–12 months, ART may be considered, depending on the couple’s goals and urgency.
Options Include:
- IUI (Intrauterine insemination)
- IVF (In vitro fertilization)
- ICSI (Intracytoplasmic sperm injection)
Varicocele repair often increases the success rate of these treatments by improving sperm DNA quality.
5.8 Managing Varicocele Recurrence
If symptoms return or semen parameters worsen, recurrence may be suspected.
A repeat scrotal ultrasound and Doppler evaluation are required.
If confirmed, a second repair—typically microsurgical—may restore improvement.
5.9 Internal Resource for Patients
Patients seeking more guidance on fertility treatment options, sperm health improvement, and recovery after varicocele surgery can explore additional resources on erectileandfertilityguide.com, where multiple male reproductive health guides are available.
6. Lifestyle Changes & Prevention
Lifestyle habits play a powerful role in determining how long sperm improves after varicocele surgery. Even after successful varicocelectomy, the testicles need a stable, healthy environment to recover fully. Sperm production takes about 74 days per cycle, so anything that affects hormones, circulation, oxidative stress, or scrotal temperature can extend the recovery timeline.
Below are the most clinically important lifestyle strategies I recommend to patients after surgery. These can significantly enhance semen parameters and shorten the time to fertility improvement.
6.1 Protect the Testicles From Heat Exposure
Heat is one of the biggest disruptors of sperm production.
Avoid:
- Hot tubs
- Saunas
- Steam rooms
- Heating pads
- Prolonged hot showers
- Keeping laptops on the lap
- Tight underwear or jeans
Why it matters
Reducing heat helps stabilize testicular temperature, which accelerates motility and DNA recovery.
6.2 Switch to Supportive, Breathable Underwear
For the first few weeks after surgery, supportive underwear helps healing.
After recovery, choose:
- Cotton boxers
- Loose-fitting breathable materials
This reduces scrotal warmth and improves circulation, benefiting sperm morphology and motility.
6.3 Quit Smoking Completely
Smoking increases oxidative stress dramatically.
It affects:
- Sperm DNA fragmentation
- Motility
- Testosterone levels
- Blood flow to testicles
Men who quit smoking often see faster and better postoperative sperm improvement.
6.4 Limit Alcohol Consumption
Alcohol affects liver metabolism, testosterone production, and sperm formation.
Moderate or avoid alcohol for at least 3 months after surgery to support optimal recovery.
6.5 Maintain a Healthy Weight
Obesity increases estrogen, lowers testosterone, and contributes to inflammation—all of which delay sperm recovery.
Tips:
- Include daily walks
- Add moderate exercise (not excessive cycling or weightlifting immediately after surgery)
- Follow a balanced diet rich in antioxidants
Weight optimization enhances the hormonal environment required for better spermatogenesis.
6.6 Improve Sleep Quality
Poor sleep lowers testosterone by up to 10–15%, directly impacting sperm production.
Sleep goals:
- 7–8 hours per night
- Maintain consistent sleep schedule
- Avoid screens before bedtime
- Reduce caffeine late in the day
Better sleep equals better hormonal balance.
6.7 Manage Stress Effectively
Stress increases cortisol, which suppresses testosterone and impairs spermatogenesis.
Evidence-based stress reduction methods:
- Deep breathing exercises
- Yoga
- Meditation
- Light outdoor activities
- Counseling or therapy when needed
Reducing stress supports both mental health and reproductive health.
6.8 Balanced Diet for Fertility Recovery
Foods rich in antioxidants and polyphenols improve sperm motility, integrity, and count.
Fertility-boosting foods:
- Citrus fruits
- Berries
- Spinach
- Walnuts
- Pumpkin seeds
- Avocados
- Olive oil
- Oily fish (sardines, salmon)
- Beans & lentils
These help combat oxidative stress and accelerate recovery after varicocelectomy.
6.9 Safe Sexual Activity During Recovery
In the first 1–2 weeks after surgery, avoid sexual intercourse or ejaculation to prevent discomfort or strain.
After this period, normal sexual activity is safe and does not affect surgical results or sperm improvement.
6.10 Regular Semen Testing & Follow-Up
Lifestyle changes only work when combined with proper monitoring.
Recommended schedule:
- 3 months
- 6 months
- 9–12 months
Follow-up ensures early detection of delayed recovery or varicocele recurrence.
6.11 Additional Preventive Care
- Avoid heavy lifting for at least 4 weeks
- Keep surgical area dry and clean
- Attend all postoperative appointments
- Use supportive underwear during early recovery
- Avoid strenuous gym workouts initially
These steps support proper healing and create the conditions needed for the testicles to restart healthy sperm production.
6.12 Internal Link for Continued Education
For more guidance on postoperative fertility care, improving sperm quality naturally, and managing male reproductive health, readers can explore expert articles on erectileandfertilityguide.com, where detailed lifestyle and fertility improvement guides are available.
Conclusion
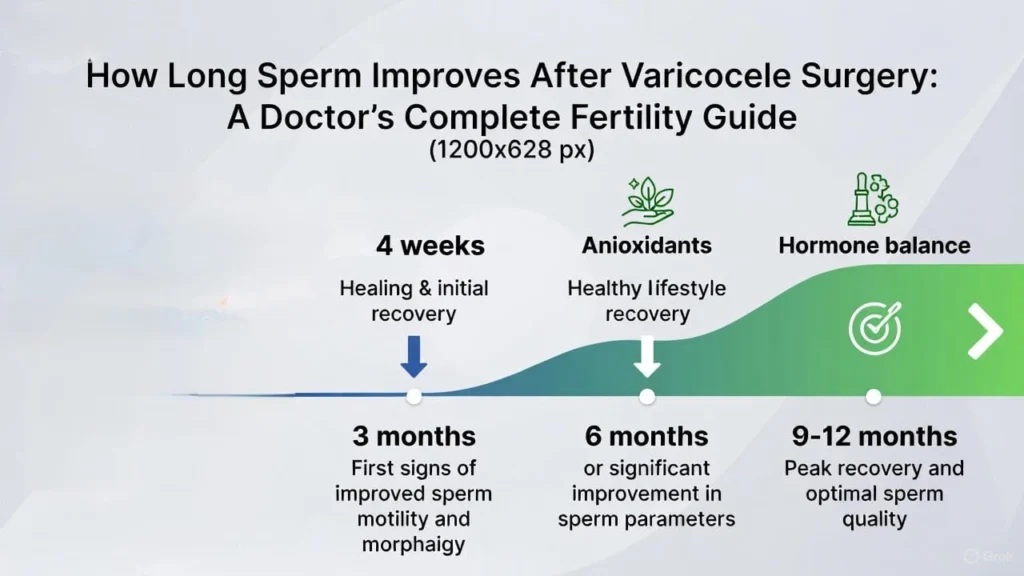
Understanding how long sperm improves after varicocele surgery allows patients and couples to plan their fertility journey with clarity and realistic expectations. Varicocelectomy is one of the most effective treatments for male infertility caused by varicocele, but sperm improvement follows a gradual biological timeline rather than immediate change. As a clinician, I remind patients that healing takes time—but improvement does happen for the majority of men.
- Summary of the Improvement Timeline
✔ First 0–4 Weeks:
Healing of the surgical site begins. No changes in semen parameters yet.
Pain, swelling, or mild discomfort may occur.
✔ 3 Months:
The first noticeable improvements often appear:
- Better motility
- Improved morphology
- Reduction in sperm DNA fragmentation
This aligns with one full spermatogenesis cycle.
✔ 6 Months:
Most men see significant improvement by this time if they maintain healthy lifestyle habits, antioxidants, and hormonal balance.
Count, motility, and DNA integrity continue improving.
✔ 9–12 Months:
Peak improvement is typically reached.
For men with severe damage, this period shows the most meaningful gains.
- Factors That Speed Up Recovery
Men who:
- Quit smoking
- Avoid heat exposure
- Take antioxidants
- Maintain a healthy weight
- Follow hormone optimization
- Manage stress
- Eat a fertility-balanced diet
usually see faster enhancement in semen parameters
- When to Seek Further Help
If sperm parameters do not improve by 6–9 months, additional evaluation is recommended to rule out:
- Varicocele recurrence
- Persistent hormonal imbalance
- Severe DNA fragmentation
- Underlying testicular dysfunction
Timely follow-up ensures that supportive treatments—such as antioxidants, Clomiphene, hCG therapy, or ART options like IUI/IVF/ICSI—can be introduced earl
- The Most Important Message for Patients
Sperm improvement is not an overnight process. It reflects biological healing, hormonal stabilization, and the restart of healthy sperm production cycles.
With proper treatment, lifestyle modification, antioxidant support, and regular monitoring, most men experience meaningful improvement in fertility within 3 to 12 months after surgery.
Your recovery journey is personal—and with evidence-based guidance, you can optimize your outcomes and increase your chances of natural conception.
FAQs
- How long does it take for sperm to improve after varicocele surgery?
Most men start seeing measurable improvement within 3 months, but optimal sperm quality—including count, motility, and morphology—usually improves by 6 months after varicocele surgery. In severe cases, full recovery may take up to 12 months.
- Does every man experience sperm improvement after varicocele repair?
Not everyone responds the same way. Studies show that 60–85% of men experience improved semen parameters after surgery, and 30–50% report improved natural pregnancy rates. Factors like varicocele grade, age, and pre-surgery sperm levels influence recovery.
- Is sperm improvement faster after microsurgical varicocele repair?
Yes. Microsurgical varicocelectomy typically results in faster and more consistent sperm improvement compared to laparoscopic or embolization methods because it preserves testicular vessels and reduces recurrence risk.
- Can sperm worsen initially after varicocele surgery?
In some men, sperm parameters may temporarily decline in the first 4–8 weeks due to post-surgical inflammation. This is normal. Improvement usually begins once healing stabilizes.
- How long should we wait before trying to conceive after varicocele surgery?
Most couples are advised to start trying after 3 months, when early sperm improvement becomes visible. However, peak fertility potential is typically achieved around 6 months.
- Does varicocele surgery improve testosterone along with sperm?
Yes. Many men experience a 15–25% increase in testosterone within 3–6 months after varicocelectomy. Higher testosterone can further boost libido, erections, and sperm production.
- What if semen parameters do not improve after 6 months?
If there is minimal improvement by 6 months, we re-evaluate for:
- Hormonal issues (low testosterone, high prolactin, thyroid imbalance)
- Lifestyle factors (smoking, heat exposure, obesity)
- Genetic conditions (Y-chromosome microdeletion)
- Incorrect surgical technique or recurrence
In such cases, treatment options on your website—like lifestyle optimization, supplements, and assisted reproduction—can be helpful. You can internally link to content on https://erectileandfertilityguide.com for deeper guidance.
- Can supplements speed up sperm recovery after varicocele surgery?
Yes. Antioxidants can accelerate healing and sperm regeneration. I often recommend:
- CoQ10 (200–300 mg/day)
- Vitamin C & E
- Zinc
- L-Carnitine
- Omega-3 fatty acids
These help reduce oxidative stress caused by years of varicocele-induced heat damage.
- How long does it take for sperm morphology to improve after varicocele repair?
Morphology (shape) often takes the longest to improve. Noticeable progress usually occurs around 3–6 months, with maximum improvement at 9–12 months.
- Does semen volume improve after varicocele surgery?
Semen volume may improve slightly, but varicocelectomy primarily enhances count, motility, and morphology, not volume. Low volume usually has other causes, such as hormonal imbalance or ejaculatory duct issues.
📚 References
| # | Study / Review | What It Shows / Key Findings |
| 1 | Khan A, Shujaa I, Gul T, Imran A, Hussain M. The Role of Varicocelectomy on Semen Parameters and Fertility. J Saidu Med Coll. 2019. link (jsmc.pk) | Prospective study of 98 men showing significant increases in sperm count at 3 and 6 months post‑varicocelectomy. |
| 2 | Systematic review & meta‑analysis: The benefits of varicocele repair for achieving pregnancy in male infertility: A systematic review and meta-analysis. 2020. Available via PubMed: link (PubMed) | Analysis of 31 articles showing varicocele repair increases pregnancy and live birth rates, regardless of initial semen parameters. |
| 3 | Prospective observational study: Evaluation of Sperm Count Improvement Following Microsurgical Varicocelectomy. (2024–2025). Available via PubMed. link (PubMed) | Reported significant increase in sperm count at 3 months post‑surgery in men with clinical varicocele. |
| 4 | Review: Summary evidence on the effects of varicocele treatment to improve natural fertility in subfertile men. (2015) — PMC. link (PubMed) | Pooled data from many studies shows significant improvement in sperm concentration and motility after varicocele repair, plus reduction in sperm DNA damage / oxidative stress. |
| 5 | Clinical review: Microsurgical Management of Male Infertility: Compelling Evidence That Collaboration with Qualified Male Reproductive Urologists Enhances ART Outcomes. (2021) — MDPI. link (MDPI) | Indicates that varicocele negatively impacts sperm DNA integrity, and repair significantly improves DNA fragmentation and sperm quality. |
| 6 | Systematic review (Oct 2023): Impact of Varicocele Repair on Assisted Reproductive Technique Outcomes in Infertile Men. PubMed. link (PubMed) | Shows varicocele repair before ICSI improves fertilization rate, clinical pregnancy rate, and live‑birth rate compared to no repair. |
| 7 | Retrospective study: Microsurgical varicocelectomy efficacy in treatment of men with primary and secondary infertility (Archivio Italiano di Urologia e Andrologia). link (PAGEPress Journals) | Demonstrates significant improvements in total motile sperm count and progressive motility, especially in men with primary infertility. |
| 8 | Short‑communication: Impact of Varicocele Cure on Spermogram Parameters and Fertility. Mathews Journal of Surgery. 2023. link (mathewsopenaccess.com) | Recent evidence supporting improvement of semen parameters (count and motility) after varicocele repair in varied patient populations. |